Translate this page into:
Psychosis as Primary Presentation of Neurological Disorders

*Corresponding author: Therissa Benerji, Department of Psychiatry, Dr. Pinnamaneni Siddhartha Institute of Medical Sciences and Research Foundation, Vijayawada, Andhra Pradesh, India teresabenerji@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kodali M, Benerji T, Lella S, Devarapalli S, Jahan N, Pallekona R, et al. Psychosis as Primary Presentation of Neurological Disorders. Bengal J Psychiatry. doi: 10.25259/BJPSY_12_2024
Abstract
Psychosis can be a primary manifestation of various neurological disorders, often leading to misdiagnosis and inappropriate treatment. This case series highlights the importance of recognizing psychosis as a potential presentation of underlying neurological conditions, particularly in patients with unusual or resistant psychiatric symptoms. We present five cases where psychosis was the primary symptom of conditions: leukodystrophy, tuberous sclerosis, meningioma, subacute subdural hemorrhage, and anti-N-Methyl-D-Aspartate (anti-NMDA) receptor encephalitis. Early recognition, appropriate imaging, and neurological consultation were crucial in diagnosing and managing these conditions, resulting in a better prognosis for patients. This case series emphasizes the need for a high index of suspicion, particularly when patients present with atypical psychiatric symptoms along with neurological findings.
Keywords
Anti-NMDA receptor encephalitis
Leukodystrophy
Meningioma
Secondary psychosis
Subdural hemorrhage
Tuberous sclerosis
INTRODUCTION
Psychosis, characterized by delusions, hallucinations, and impaired reality testing, is traditionally regarded as a psychiatric disorder. However, a variety of neurological conditions may present with psychosis as their primary symptom, leading to significant diagnostic challenges. These cases often involve complex, multi-system disorders that can be easily overlooked if not carefully considered. Misdiagnosis may lead to prolonged treatment with psychotropic medications without addressing the underlying neurological cause, resulting in delayed diagnosis and worsening of the condition.
This case series aims to underscore the importance of considering neurological disorders in the differential diagnosis of psychosis, particularly when the clinical picture does not align with typical psychiatric conditions or when there is treatment resistance. We present five cases where psychosis was the primary presentation of the following neurological conditions: leukodystrophy, tuberous sclerosis, meningioma, subacute subdural hemorrhage, and anti-NMDA receptor encephalitis.
CASE SERIES
Case 1: Leukodystrophy Presenting as Psychosis
A 31-year-old male, previously diagnosed with a severe depressive episode with psychotic symptoms, reported no improvement after 2 years of treatment with antidepressants and antipsychotics and presented with a history of fearfulness, suspiciousness, inappropriate smiling, decreased self-care, and disturbed sleep. Family history revealed hemiparesis in the elder sister along with symptoms of inappropriate smiling, self-muttering, recurrent headaches, and seizures. Her MRI brain showed acute infarct in the left frontal region, chronic lacunar infarcts in bilateral capsuloganglionic regions, the right corona radiata, and bilateral fronto-parietal regions along with small vessel ischemic changes, who died of status epilepticus subsequently. The patient’s lack of improvement despite 2 years of psychotropic treatment, coupled with a family history of neurological symptoms and MRI abnormalities, raised suspicion of an underlying neurological disorder, warranting neuroimaging workup.
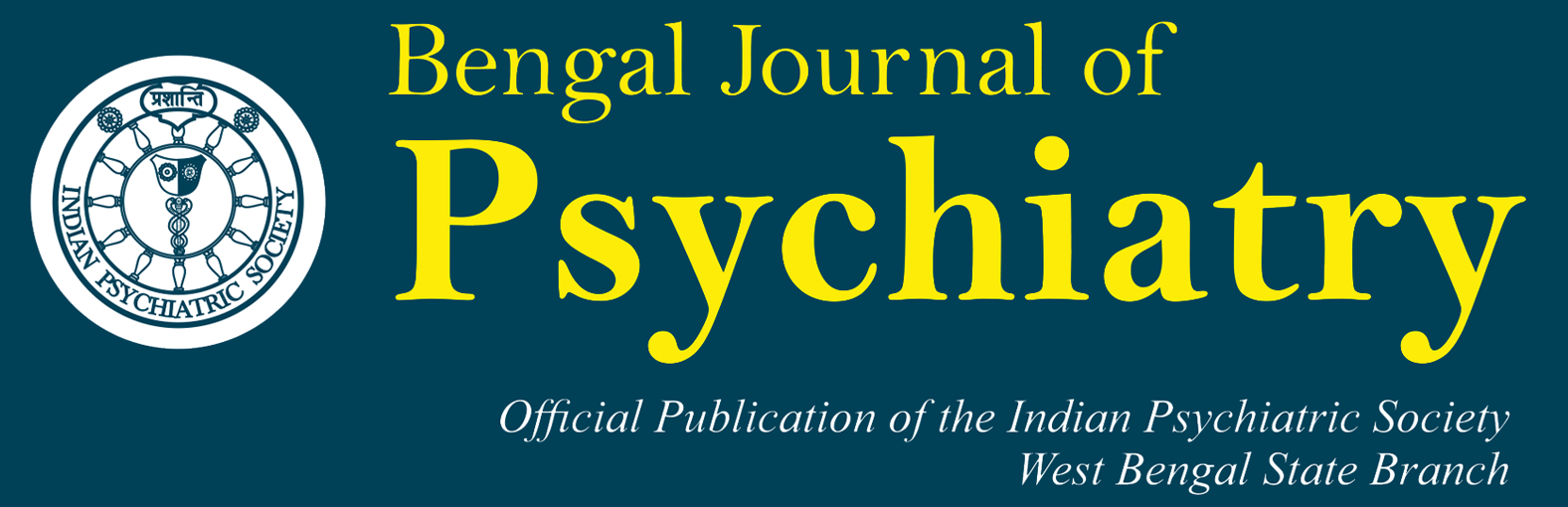
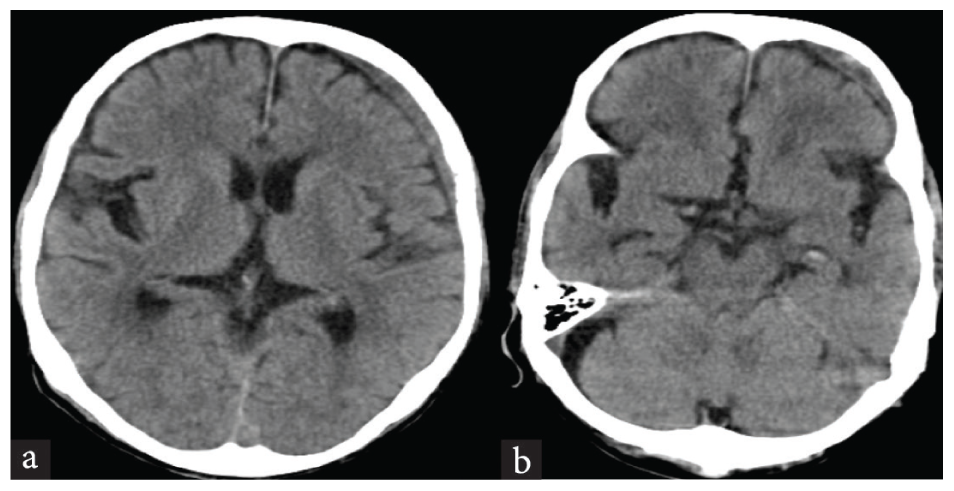
The patient’s MRI brain revealed extensive leukoencephalopathy involving the frontoparietal white matter [Figure 1a] and deep gray matter nuclei [Figure 1b], suggestive of metachromatic leukodystrophy (MLD). The patient was switched to trihexyphenidyl and olanzapine, which led to significant improvement in his symptoms. This case highlights the importance of considering neurological causes like leukodystrophy when psychiatric symptoms are treatment-resistant and suggests a need for thorough neurological evaluation.
- MRI brain: Leukoencephalopathy involving the a) Frontoparietal white matter, b) deep gray matter.
Case 2: Tuberous Sclerosis Presenting as Psychosis
A 50-year-old man with a history of mild intellectual disability presented with a 1-year history of irritability, suspiciousness, self-muttering, and socio-occupational decline. His psychiatric symptoms were accompanied by auditory hallucinations and delusions of persecution. Notably, the patient had a long history of generalized tonic-clonic seizures, starting at the age of 2.
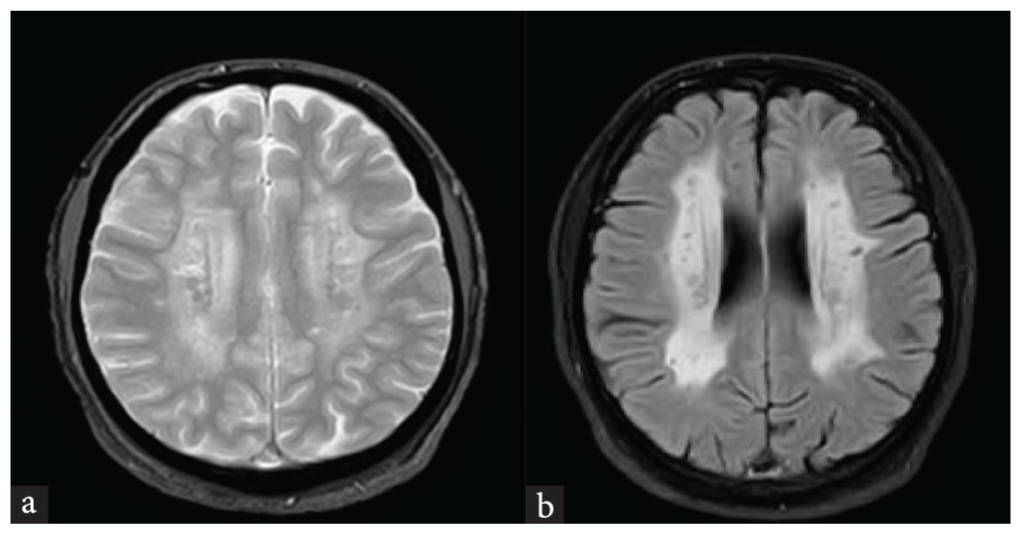
Physical examination revealed cutaneous features such as facial angiofibromas [Figure 2a], hypomelanotic macules, and Koenen’s tumors [Figure 2b]. The patient’s characteristic cutaneous features and longstanding generalized tonic-clonic seizures strongly suggested tuberous sclerosis, warranting neuroimaging to confirm the diagnosis. CT brain showed multiple calcified subependymal nodules [Figure 2c] and subcortical calcifications [Figure 2d], confirming the diagnosis of tuberous sclerosis. The patient was diagnosed with an organic schizophrenia-like a disorder due to tuberous sclerosis and managed with risperidone. Although rare, this case emphasizes the importance of considering tuberous sclerosis in patients presenting with characteristic skin lesions, a history of seizures, and psychosis.
- (a) Facial angiofibromas, (b) Koenen’s tumor over great toe, CT brain: (c) calcified subependymal nodules around lateral ventricles, and (d) subcortical calcifications.
Case 3: Meningioma Presenting as Psychosis
A 32-year-old male presented to the psychiatry outpatient department with complaints of headache, blurred vision, irritability, fearfulness, and delusions of persecution. His psychiatric symptoms were accompanied by a history of visual disturbances, including left ptosis. Neurological examination revealed left oculomotor nerve palsy and mild right-sided weakness. The patient’s unexplained headache, visual disturbances, and focal neurological deficits raised suspicion of an underlying neurological disorder, warranting neuroimaging for further evaluation.
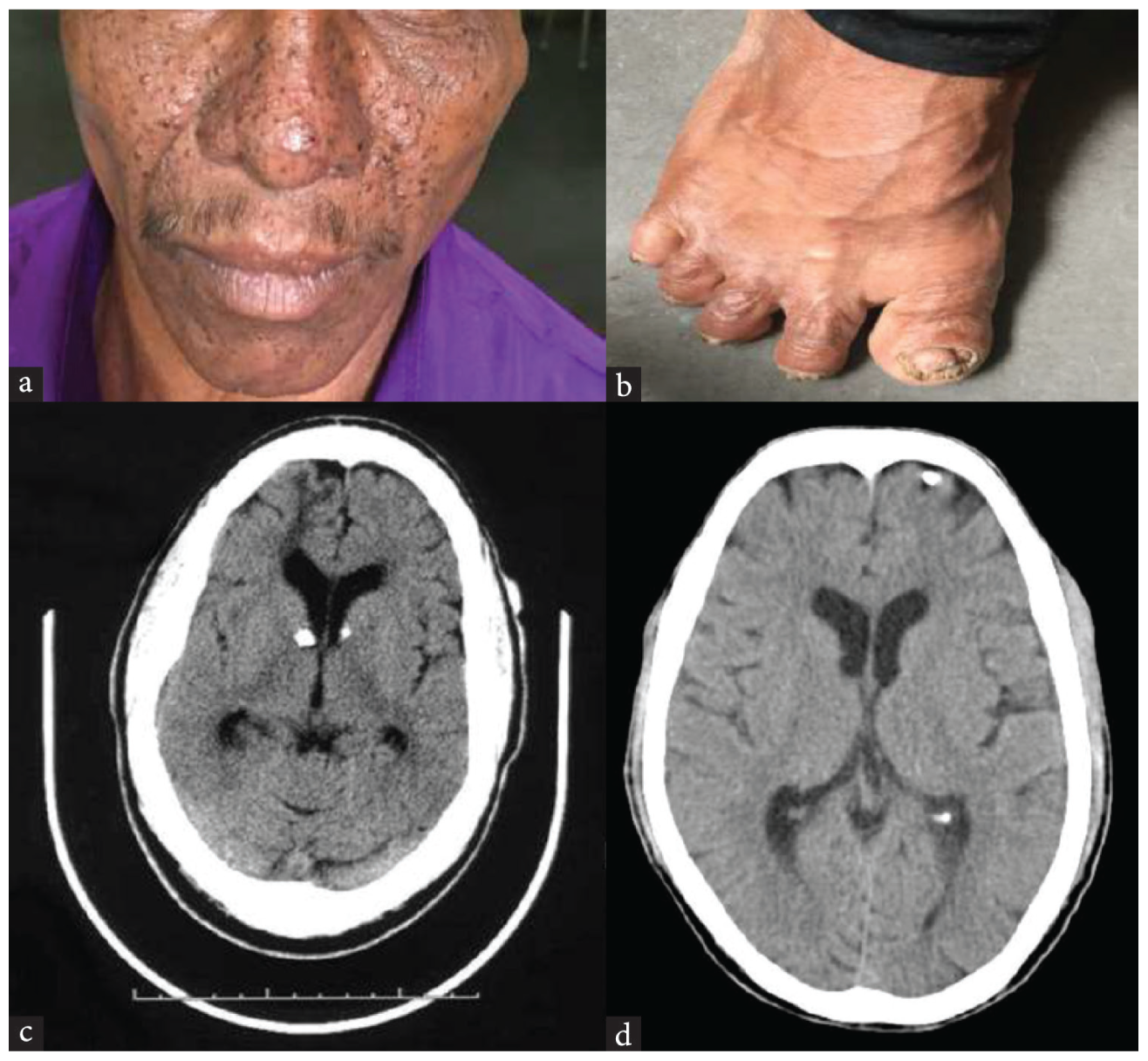
CT brain showed an aggressive skull base meningioma with extension into the left temporal region [Figure 3a] and sphenoid wing [Figure 3b]. The patient was referred for neurosurgical consultation and diagnosed with meningioma with organic schizophrenia-like disorder. This case demonstrates that meningiomas, while typically asymptomatic, can present with psychiatric symptoms such as psychosis when they involve the frontal or temporal lobes.
- CT brain: a) Skull base meningioma in the left temporal region, b) skull base meningioma showing extension into the left sphenoid wing.
Case 4: Subacute Subdural Hemorrhage Presenting as Psychosis
An 85-year-old man presented with irritability, diffuse, dull headache, auditory hallucinations, and delusions of persecution. His symptoms developed over the past 10 days, and he had a recent history of sleep disturbances. Despite a lack of significant trauma, the patient exhibited signs of cognitive impairment, including poor concentration and recent memory loss. The patient’s sudden-onset cognitive impairment and acute psychiatric symptoms raised suspicion of an underlying neurological disorder, warranting further investigations to identify potential causes.
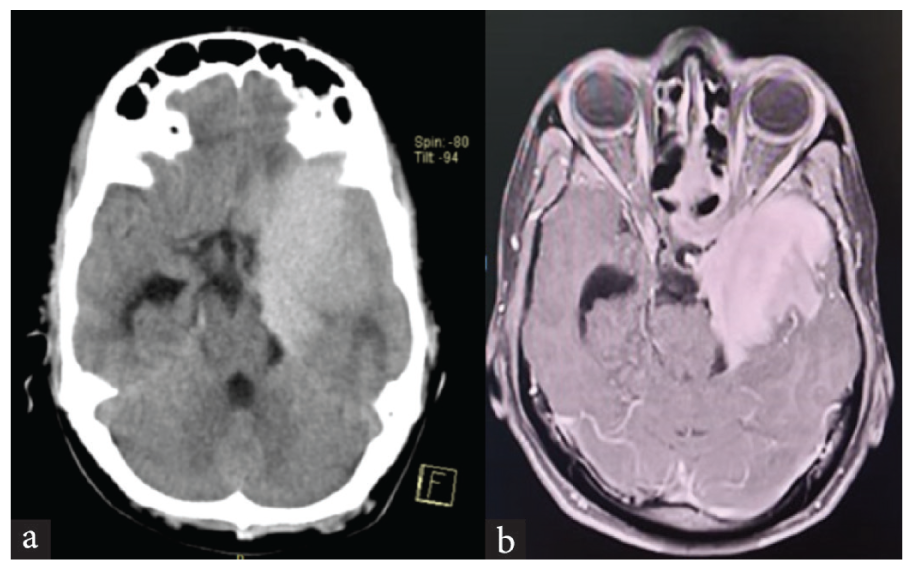
CT brain showed a subacute subdural hemorrhage in the left cerebral convexity [Figure 4a], along with lacunar infarcts in the midbrain and pons [Figure 4b]. The patient was diagnosed with left subacute subdural hematoma, which was referred for neurosurgical management. This case underscores the importance of considering subdural hematoma in elderly patients presenting with acute psychiatric symptoms, especially when there is no clear history of trauma.
- CT brain: a) Subdural hemorrhage in the left cerebral convexity, b) lacunar infarcts in the midbrain and pons.
Case 5: Anti-NMDA Receptor Encephalitis with Psychosis
A 39-year-old male, following a viral fever with chills and rigors, developed psychosis characterized by irrelevant speech, delusions of persecution, and agitation. His condition deteriorated rapidly, with high fever, seizures, slurred speech, and an inability to recognize family members. As the patient developed psychosis following fever and rapidly deteriorated with seizures and slurred speech, an underlying neurological disorder was suspected, warranting urgent investigations for possible causes.
MRI brain revealed restricted diffusion in the bilateral thalamus [Figure 5], suggestive of viral encephalitis. Cerebrospinal fluid (CSF) testing was positive for anti-NMDA receptor antibodies, confirming the diagnosis of anti-NMDA receptor encephalitis. The patient was treated with antiviral therapy, anticonvulsants, and corticosteroids, leading to gradual improvement. This case highlights the importance of considering autoimmune encephalitis in the differential diagnosis of acute psychosis, particularly when accompanied by neurological signs such as seizures and altered consciousness.
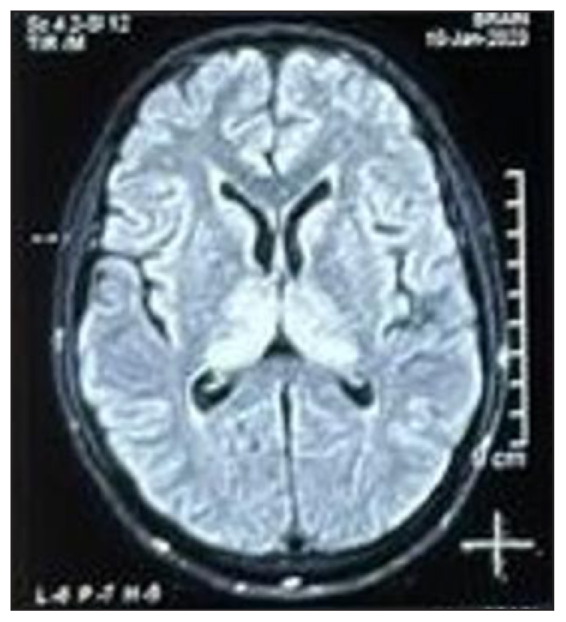
- MRI brain: Restricted diffusion in the bilateral thalamus.
DISCUSSION
Psychosis is commonly associated with primary psychiatric disorders, but several neurological conditions can present with psychosis as the primary symptom.1,2 The five cases in this series illustrate a range of neurological disorders—leukodystrophy, tuberous sclerosis, meningioma, subacute subdural hemorrhage, and anti-NMDA receptor encephalitis—that can manifest with psychiatric symptoms, complicating diagnosis and management. These conditions highlight the need for a high degree of clinical suspicion when faced with atypical psychiatric presentations and resistance to treatment, especially in patients with neurological signs or an unclear etiology.
Leukodystrophies, like MLD, often present with cognitive decline and psychiatric symptoms, which can be misinterpreted as primary psychiatric illness. Early imaging, including MRI, is crucial in identifying the white matter changes characteristic of these disorders.3 Tuberous sclerosis can present with psychosis due to the impact of cortical tubers on limbic structures. The hallmark of this disorder includes skin manifestations and seizures, which can aid in diagnosis when psychiatric symptoms predominate.4,5
Meningiomas, while typically benign, can cause significant neurological deficits and psychiatric symptoms when located in areas such as the frontal or temporal lobes.6,7 Similarly, subdural hematomas, especially in the elderly, can lead to sudden psychiatric disturbances, including delusions and cognitive impairment.8 Finally, anti-NMDA receptor encephalitis, a potentially reversible cause of psychosis, highlights the role of autoimmune processes in psychiatric presentations.9 The importance of early diagnosis and treatment, particularly with regard to autoimmune encephalitis, cannot be overstated, as timely intervention can result in significant recovery.10
In conclusion, this case series emphasizes the necessity of a comprehensive clinical evaluation in patients presenting with psychosis, especially when accompanied by neurological symptoms or when the patient is unresponsive to conventional psychiatric treatment. A multidisciplinary approach involving both neurologists and psychiatrists is often crucial in ensuring the proper diagnosis and management of these complex cases.
CONCLUSION
Psychosis as a primary presentation of neurological disorders is a diagnostic challenge that requires a high index of suspicion. The cases presented in this series underscore the importance of considering neurological causes, including leukodystrophy, tuberous sclerosis, meningioma, subacute subdural hemorrhage, and anti-NMDA receptor encephalitis, when encountering psychiatric symptoms that are resistant to conventional treatment or lack clear psychiatric etiology. Early recognition through appropriate imaging and neurological consultation is essential for accurate diagnosis and effective management, leading to improved patient outcomes.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
REFERENCES
- Secondary Psychoses: An Update. World Psychiatry. 2013;12:4-15.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Metachromatic leukodystrophy: Diagnosis, modeling, and treatment approaches. Front Med (Lausanne). 2020;7:576221.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Tuberous sclerosis: its neurological and neuropsychiatric aspects and a case report. Kerala J Psychiatry. 2018;31:30-37.
- [CrossRef] [PubMed] [Google Scholar]
- Neuropsychiatric manifestations of tuberous sclerosis and Management Options: A Narrative Review. Prim Care Companion CNS Disord. 2024;26:22nr03481.
- [CrossRef] [PubMed] [Google Scholar]
- Secondary psychosis due to meningioma. A review about a case. J Neuroeuropsychiatry. 2021;59:72-83.
- [Google Scholar]
- Meningioma and Psychiatric Symptoms: An Individual Patient Data Analysis. Asian J Psychiatr. 2019;42:94-103.
- [CrossRef] [PubMed] [Google Scholar]
- Psychiatric manifestation of Chronic Subdural Hematoma: The Unfolding of mystery in a Homeless Patient. Indian J Psychol Med. 2015;37:239-42.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Anti-NMDA Receptor Encephalitis, Autoimmunity, and Psychosis. Schizophr Res. 2016;176:36-40.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Psychiatric presentation of anti-NMDA receptor encephalitis. Front Neurol. 2019;10:1086.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]